SAN DIEGO — The head of the largest long-term and senior care trade group didn’t sugarcoat the current state of affairs Monday. In his 25 years in the field, this might be the most challenging climate he’s ever seen, he said.
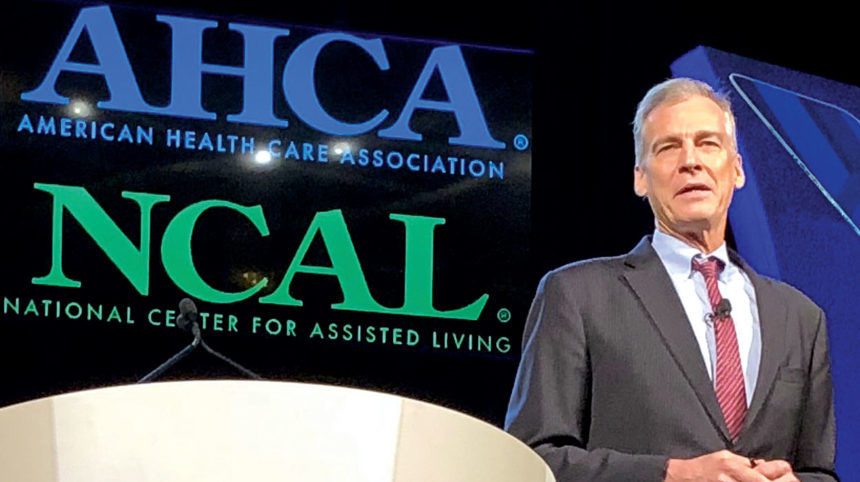
“I’m always the calming voice that says, ‘Hey, we say that every year. This probably isn’t the toughest year. We’re going to be fine,’” Mark Parkinson, president and CEO of the American Health Care Association, told attendees Monday at the group’s 69th annual convention. “But this year, I can’t really be the calming voice. I do think we’re going to be just fine, but I really do think this is our toughest time, ever.”
The reasons, he said, include everything from struggles finding workers, to changing payment models, dipping occupancy rates and declining lengths of stay. That’s all on top of the usual pressures squeezing SNFs on an annual basis, from inadequate Medicaid reimbursement rates to overburdensome regulations.
He noted that many observers are predicting that skilled nursing is in trouble — that the model is obsolete, independent owners won’t be able to navigate new payment models and that nursing homes may not survive the future. “The question that we face is are we going to let these negative ideas and predictions about us be true, or are we going to overcome them?”
He gave operators three ideas for handling this toughest time:
(1) Get ready for PDPM: “The Patient Driven Payment Model is not a tinkering of our payment system. It is a completely new system,” he said, later adding: “Folks that [prepare and implement it properly] are going to do very well and folks that don’t get prepared are not going to do well.”
AHCA created a new toolkit to simplify the new payment model, which it was sharing with members at exclusive convention sessions Sunday and Wednesday. In January, association reps will head to nearly every state to do full-day training, along with further toolkit updates to follow.
(2) Continue to get better and keep getting better: “It’s very clear that both on the SNF and on the [assisted living] side, we’re already doing a good job. These are the things that CMS measures for quality outcomes, and on virtually all of them, and certainly all of the one that matter, we’re making a huge success at getting better on all of these QMs. But, we have to keep getting better and better. That’s what the future is all about.”
(3) Get active: “Over 65% of our reimbursement on the SNF side is Medicare and Medicaid. On the AL side, an increasing number of people are involved in home and community-based services. If we’re not very, very involved politically, we won’t win.”
In other convention related news:
- Lois McCaskey, the VP of labor management at Genesis Health Care, prepped providers on what to do if audited under the new Payroll Based Journal reporting system. She warned nursing homes that auditors may seek a laundry list of information, with only five business days to upload the data requested.
“The first thing that you need to do when you get the audit, besides panic, is request access to the FTP site in order to upload your data,” she said, noting that Genesis has had to submit payroll records for 438 centers and has already been subject to audits at two of its smaller facilities.
She said access to the FTP site can be acquired by emailing [email protected]. Providers also can consult the help desk at [email protected] or (800) 339-9313 for data submission issues, she added.
- Recruitment and retention of workers was a popular topic Monday at the convention.
“I was just in a meeting with state execs, both skilled nursing and assisted living, and about 70% of discussion was about staffing challenges,” said Lyn Bentley, Vice President, Quality and Regulatory Affairs for AHCA, while performing moderating duties for an afternoon session on trends in skilled nursing and post-acute care. “They were also saying nurses are coming out of nursing school not being prepared to take care of patients the way they’re supposed to.”
Low national unemployment figures, the push for a $15 per hour minimum wage in some areas and bad publicity from the mainstream press about Payroll-Based Journal processes also were top workforce-related worries.
Bentley identified additional other trends to keep an eye on: increased caregiving demands in the behavioral health area and preparation for the implementation of Phase 3 of the Requirements of Participation in November 2019.
“QAPI programs will be inspected in Phase 3 and you need to be prepared for that,” Bentley said. “Another thing is compliance and ethics programs.”
She added, however, that “until we see those interpretive guidelines (from CMS), we don’t know what the expectations are. They can certainly provide more clarity.”
Along those lines, session panelist Lina Dureza, an administrator for Hughes Health and Rehabilitation, reminded the overlow crowd that improving workforces starts at the top.
“Management should do rounds at the beginning or end of shifts to thank staff, ask their opinions and acknowledge their contribution,” she said.
“The burden is on leadership and management. We can never expect our staff to do what we want them to do if we do not set a good example,” she added. “We can talk, talk, talk. But if we don’t do what we say, we will never be successful.”




