Critics wasted little time expressing their displeasure with the government’s final nursing home payment rule for fiscal 2025 after it was released late Wednesday afternoon.
While nudging up Medicare Part A pay rates from a proposed 4.1% to 4.2%, the final rule also codified broader powers for regulators levying civil monetary penalties. Gaining less immediate reaction were tune-ups to value-based purchasing and quality reporting program provisions and other administrative adjustments.
“I’m disgusted. With Medicare utilization dropping to single digits in many states, the [SNF PPS pay rule] is an ‘enforcement rule’ more than a ‘payment rule,’” criticized post-acute payment expert Marc Zimmet in an email to McKnight’s Long-Term Care News. “CMS continues to adjust Medicare reimbursement as if the program exists in a vacuum by ignoring realities of a devolving revenue model.”
“Responsible” rulemaking would address data collection on Medicare Advantage utilization and payment, Medicaid cost-sharing for dual-eligible coinsurance, and SNF-specific expense variation “as opposed to destabilizing AWI updates that arbitrarily penalize thousands of providers,” added Zimmet, the CEO of Zimmet Healthcare Services Group.
“The average provider’s gross reimbursement will increase $100,000 — that fixes nothing,” he noted.
The 315-page final rule was first detailed in a McKnight’s Breaking News bulletin late Wednesday afternoon. It will be published in the Federal Register Aug. 6; it currently can be seen in unpublished form here.
While calling the Medicare rate hike helpful toward meeting “escalating needs,” the leader of the nation’s largest nursing home association ripped into regulators giving themselves expanding fining powers.
“[W]e are extremely disappointed in the Civil Monetary Penalties (CMP) policy that CMS finalized in this rule. In particular, we are deeply troubled by CMS’ statement that it is ‘expanding its ability to impose financial penalties,’ as this is a clear indication of agency overreach when it comes to enforcement,” said AHCA President and CEO Mark Parkinson in an email to McKnight’s.
Parkinson noted operators’ long-time complaint that CMPs divert resources from other needed areas, while failing to deliver “constructive support for residents or addressing root causes.”
“Excessive fines run the risk of pushing nursing homes already on the financial brink to closure, uprooting residents and staff, and putting unnecessary stress on family members as they search for new solutions for their loved ones’ care,” Parkinson added.
He said since nursing home providers and regulators share the goal of keeping residents safe, they should work more collaboratively on finding solutions, “not simply citing and fining.”
“We support the creation of incentives for nursing homes to enhance the quality of care and properly funding these facilities to ensure they have the necessary resources to provide high quality care,” Parkinson said.
Appeals for ‘the carrot’
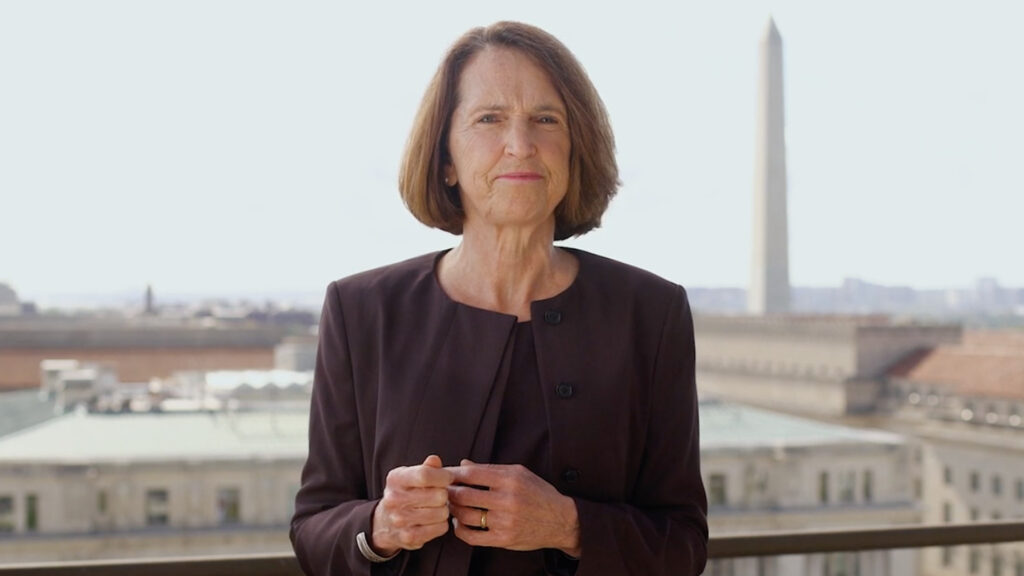
The Medicare pay increase given current operational challenges and a “very competitive labor market” is simply “insufficient,” said Katie Smith Sloan, president and CEO of LeadingAge, in a statement Wednesday.
She also expressed disappointment in the expansion of civil monetary penalty powers.
“While we agree that deficient practices must be corrected to ensure the safety and well-being of residents, CMS continually chooses to take oversight responsibility only to the point of punishment and persists in prohibiting surveyors from offering immediate guidance to correct deficient practice when it is identified,” Sloan said.
Viewing financial penalties as an effective means of quality improvement is a “mistaken belief,” she added.
She urged the administration to “refocus” and “engage in quality improvement in a productive way, choosing the carrot instead of a larger, stronger stick.”
She said the administration’s recently finalized minimum staffing rule casts a shadow over everything in long-term care.
“Real resources — including payment that recognizes the real costs, including staff wages, of providing care — must be dedicated, and meaningful solutions devised to fix long-term care’s workforce needs,” Sloan said. “America’s broken approach to funding and delivering long-term care and services must be addressed, starting with building and supporting the long-term care workforce.”





